Being a rheumatologist
A few days ago, while studying possible diagnoses for an unusual case, the on-duty resident talked about how other specialists see rheumatologists as majors in rare science. “If you cannot identify what your patient is suffering from, send them to a rheumatologist,” is the motto. Although I took the comment as a compliment, I paid no attention to it, but still decided to do a little research on its accuracy.
Just like any other patient, I started by asking Google if majors in rare science existed. As you can imagine, Google thought it was one of the many questions posed by people with nothing else to do and directed me towards other non-related-with-my-query options.
After several attempts, I found a sophisticated text titled “Why I got into Rheumatology?” published on Medscape by Dr. Stephen Paget.
Within his list of reasons, Dr. Paget mentioned the impact given by a professor and rheumatologist who, in Sherlock Holmes style, would uncover the rare cases he encountered at the hospital.
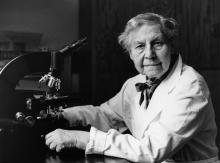
At that moment, I felt identified. I had the same experience when I was one of Antonio Iglesias Gamarra’s mentees. I also wanted to become a rare disease detective. Two additional references, one from North America and another one from German literature, supported the intern’s comment, confirming the concept was standardized.
Nevertheless, a rheumatologist is not a doctor for the rare, rather a doctor for the frequent and the painful. Our daily practice is full with patients affected by inflammatory, mechanical and soft tissue conditions which produce incapacitating chronic pain. In 2017, the Spanish Society of Rheumatology published an interesting dissertation titled “Assessment of Pain in Rheumatology.” In it, data obtained from 34 rheumatology centers shows that pain exists in 95% of the patients who attend the examination room. Pain is, in most of the cases, the main cause for consultation, and 80% comes from chronic evolution.
Rheumatologists study the particularities of pain, its distribution, intensity, repercussion and ramifications as inflammatory symptoms and signs from extra-articulations and other organs. All this in order to establish a differentiating and accurate diagnosis for every compromised condition and structure in the musculoskeletal system. The diagnoses responsible for causing the strongest, most frequent pain are inflammatory arthropathy (30%) and arthrosis (27%), followed by soft tissue rheumatism (17% including tendinitis, bursitis, myofascial syndrome) and unspecified vertebral ailments (8%). A 4.1% is also identified with neuropathic pain, which broadens the patient spectrum.
Whether a doctor for the rare, the frequent or the painful, a rheumatologist is a doctor with the knowledge necessary to develop the study, diagnosis and treatment of the inflammatory and mechanical musculoskeletal diseases, autoimmune and autoinflammatory, many of which develop a chronic pattern, and which considerably impact the morbimortality and quality of life of patients.
“You only see what you know.” JW von Goeth